
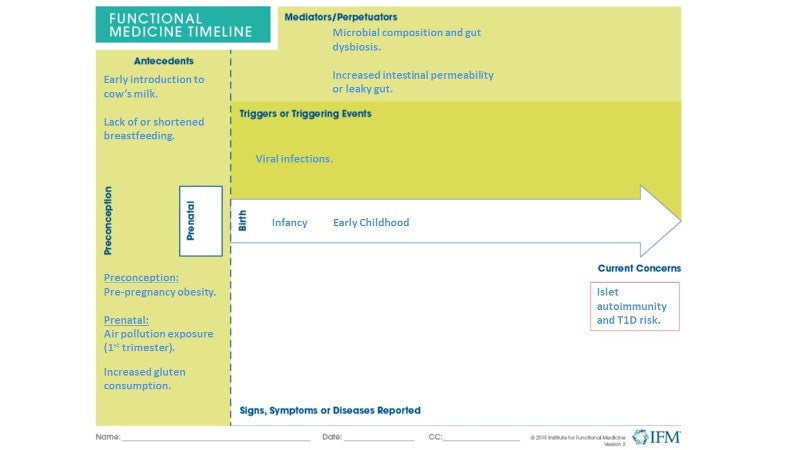
The prevalence of both autoimmune disease (AD) and pediatric chronic disease have risen dramatically in the United States over the years. A 2020 report from the Centers for Disease Control and Prevention indicates that the rate of newly diagnosed cases of the autoimmune condition type 1 diabetes (T1D) continues to rise for children and teens in the United States, with cases growing most sharply for Black, Hispanic, and Asian/Pacific Islander youths.1,2 In addition to genetic predisposition, research suggests that environmental and early-life factors may influence T1D risk and development of the disease.3
Genetics and environmental factors
Type 1 diabetes targets pancreatic islet beta cells, and the risk for and progression of this autoimmune disease includes both genetics and interactions with environmental exposures.3,4 Genetic predisposition, including HLA genotype5 and immune markers such as autoantibodies, indicates risk level for patients. Research suggests that those children with an affected first-degree relative have a tenfold higher risk of T1D compared with the general population.3 Relevant to high-risk children, observational studies suggest that T1D-associated autoantibodies may be present from the first year of life.3 Markers of islet autoimmunity are autoantibodies that appear before potential progression to T1D.6 In addition, studies indicate that immune biomarkers of T1D may be diverse, with individual at-risk patients displaying combinations of autoantibodies, T-cell profiles, and other biomarkers that suggest personalized prediction, prevention, and treatment approaches.7
From early life, whether related to maternal influences on fetal development during pregnancy or exposures during infancy and childhood, environmental factors may contribute to T1D risk and progression.3,8 The following are some examples:
- Pre-pregnancy obesity: A large cohort study found that both maternal pre-pregnancy obesity and paternal obesity rather than maternal gestational weight gain were associated with childhood-onset T1D.9
- Pollution: A 2020 retrospective cohort study investigated maternal exposures to common air pollutants and suggested that ozone (O3) exposure above 25 ppb during the first trimester of pregnancy was associated with increased pediatric diabetes risk.10
- Food antigens: Early introduction to cow’s milk and maternal gluten intake may play an important role for those children at increased risk for T1D.8,11,12 A national cohort study in Denmark (n=67,565 pregnancies) found that a child’s T1D risk increased in proportion with maternal gluten consumption during pregnancy.11
- Breastfeeding: A 2018 systematic review and meta-analysis of 31 observational studies suggested that breastfeeding may have a protective effect, with longer exclusive breastfeeding associated with reduced T1D risk.13
- Viral exposure: A large 2019 cohort study (n=1,474,535 infants) based on US data from 2001-2017 found a 33% reduction in T1D risk after the completion of the rotavirus vaccine series compared to those who did not complete the series.14
- Microbiome: Continuing research suggests that early microbiome influences, including gut dysbiosis, may also contribute to T1D risk and disease progression.3,15 A 2018 observational study investigating stool samples from mostly white, non-Hispanic children (n=783) found that children with genetic predisposition for T1D and signs of islet autoimmunity had higher levels of Streptococcus group mitis/oralis/pneumoniae species while the controls had a higher abundance of Lactobacillus rhamnosusand Bifidobacterium dentium.4 Further, the microbial composition of the children in the control group included more genes related to the fermentation and production of short-chain fatty acids.4
- Intestinal permeability: Increased intestinal permeability, commonly known as leaky gut, plays a role in autoimmune disease.16 Specifically, in individuals with genetic predisposition to autoimmunity, the upregulation of zonulin, the modulator of intercellular tight junctions and regulator of the mucosal immune response, leads to altered epithelial tight junctions and increased susceptibility to environmental triggers, potentially leading to autoimmune diseases, including T1D.17,18
Prevention strategies & clinical considerations
Research trials that investigate pharmaceutical and non-pharmaceutical prevention approaches for the development of T1D tend to focus on high-risk individuals who have a genetic predisposition as well as those patients who have diagnosed islet autoimmunity.12 These interventions and approaches may include insulin, monoclonal antibodies, vitamin D, omega-3 fatty acids, probiotics, and nicotinamide. They may also address the previously mentioned environmental exposures that impact T1D risk12 and potentially hold promise for prevention. While studies have reported inconsistent conclusions, some dietary strategies have shown positive results in reducing islet immunity rates and T1D risk.12 A 2007 observational study based on dietary intake data (n=1,770) found that omega-3 fatty acid consumption by children with increased genetic risk for T1D reduced the risk of developing islet immunity.5 A 2013 meta-analysis of cohort and case-controlled studies found that vitamin D intake during early life may have protective effects, reducing the risk of T1D.19
In an environment of increased cases of autoimmunity and pediatric chronic disease, the functional medicine model targets underlying causes and addresses those antecedents or triggers that influence the progression of autoimmune conditions such as type 1 diabetes. From preconception and prenatal care to recognizing pertinent environmental exposures and proactive approaches, in addition to insulin, functional medicine interventions implement personalized prevention or treatment strategies that can lead to better health outcomes.
Members Only Content
To continue reading please subscribe to WellnessPlus by Dr. Jess MD
Be your own best doctor with our comprehensive suite of online health coaching tools.
